Japanese Non-surgical Orthopedics Society (JNOS) aims to develop diagnosis and treatment, academia, education and research for musculoskeletal pain and intractable pain related to fascia.
Notably, in recent years, we focus on elucidation of anatomy and pathophysiology of fascia, ultrasound-guided fascia release (injection[hydrorelease], dry needling, manipulative therapy) and establishment of terminology of fascia and its related terms.
Contents
- 1.What is Non-surgical Orthopedics?
- 2.What is the definition of fascia
- 3.What are abnormal fasciae which cause any symptoms?
- 4.Diagnosis/assessment of fascia
- 5.Therapy of fascia
- 5-1 Guide for selecting the type of treatment tequniques
- 5-2 What is fascia hydrorelease?
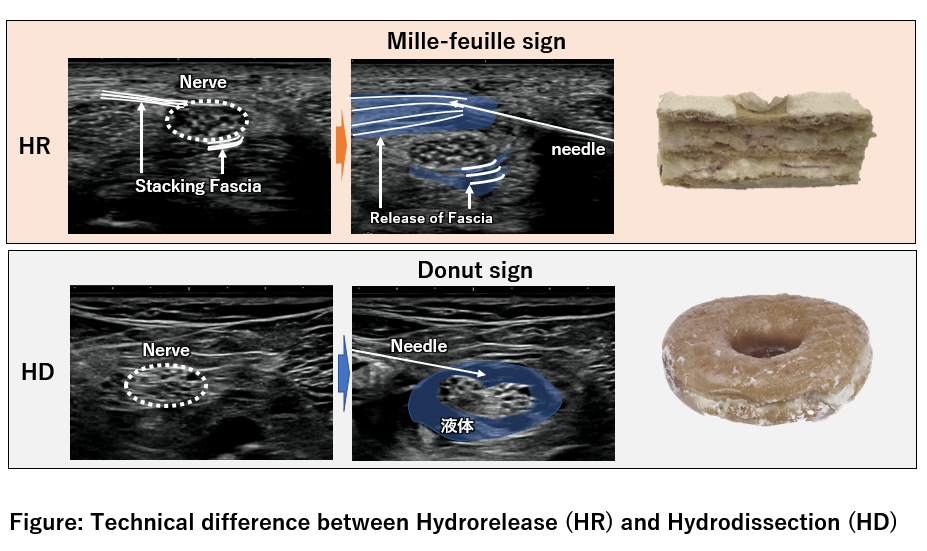
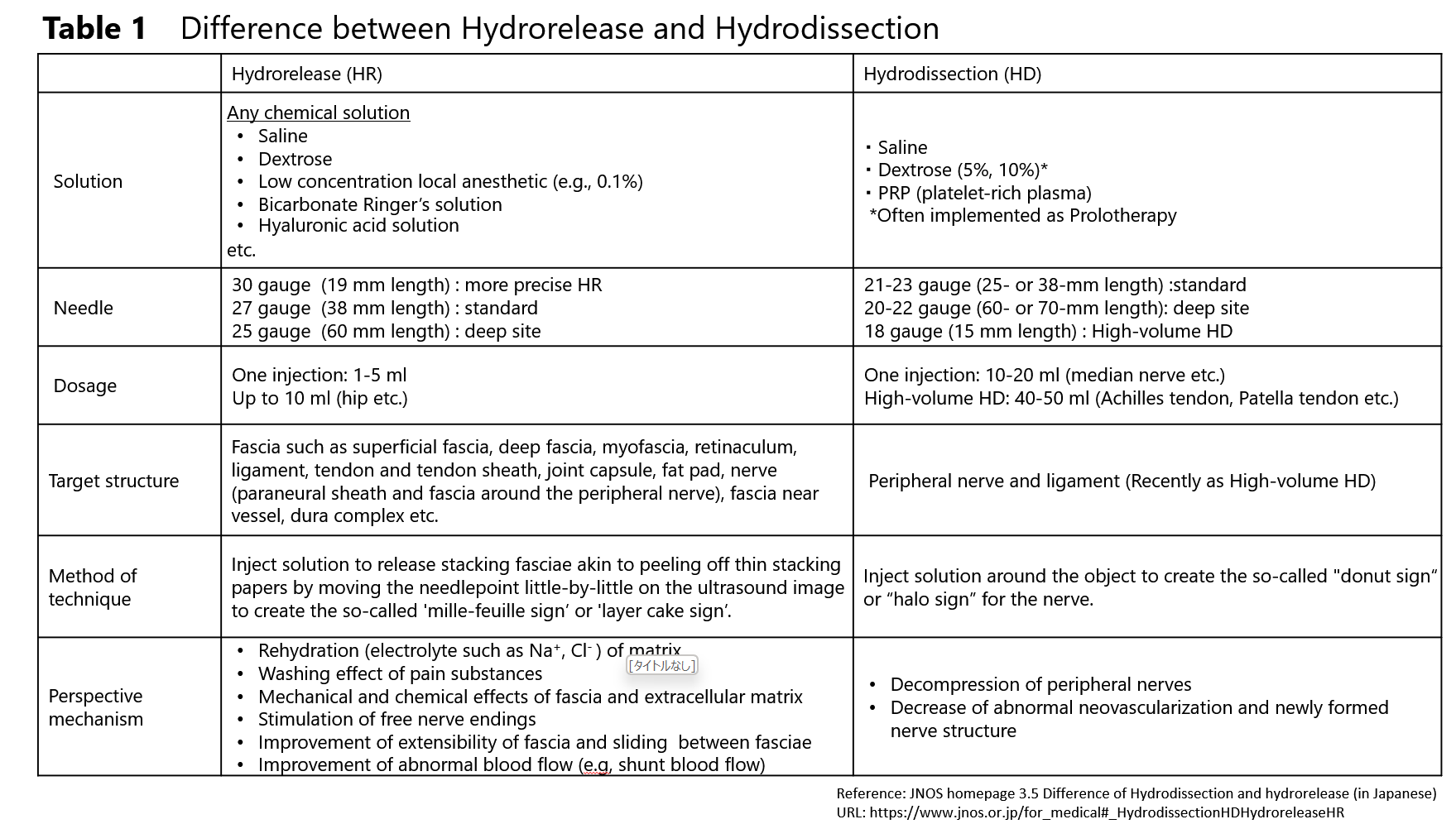
- 5-3 The difference between hydrorelease (HR) and hydrodissection (HD)
- 5-4 Comparision of targets and ultrasound signs between Hydrorelease(HR), Hydrodissection(HD), and Peripheral nerve block
- 5-5 Classifying Local Treatments: Aiming to Loosen or Tighten Tissue and Fascia
- 5-6 Hydrorelease of fibrils as of fascia, into a peripheral nerve
- 5-7 Specific examples of ultrasound-guided fascia hydrorelease
- 6. Message for multi-medical professionals
- 7. Further Information
1.What is Non-surgical Orthopedics?
JNOS defines the term of non-surgical orthopedics as a field of medicine in which medical treatment and research of musculoskeletal pain and refractory pain with less invasive treatment as possible.
2.What is the definition of fascia
The definition of fascia is under international debate. For recent examples;
- Gray’s anatomy 2015: Genetic term applied to sheaths, sheets or other dissectible masses of connective tissue that are large enough to be visible to the unaided eye. Including connective tissue between skin and muscle, surrounding muscles, viscera, linking them together as neurovascular bundles, and related structure. Fascia is no longer included in the Terminologia Anatomica (TA).
- FRC(fascia research congress) 2012: Fibrous collagenous tissues which are part of a body-wide tensional force transmission system”.
- Carla Stecco et al.: a sheath, a sheet, or any number of other dissectible aggregations of connective tissue that forms beneath the skin to attach, enclose, and separates muscles and other internal organs
(Stecco C, 5th FRC, 2015 and Stecco C, Schleip R: J body move ther. 2016.)
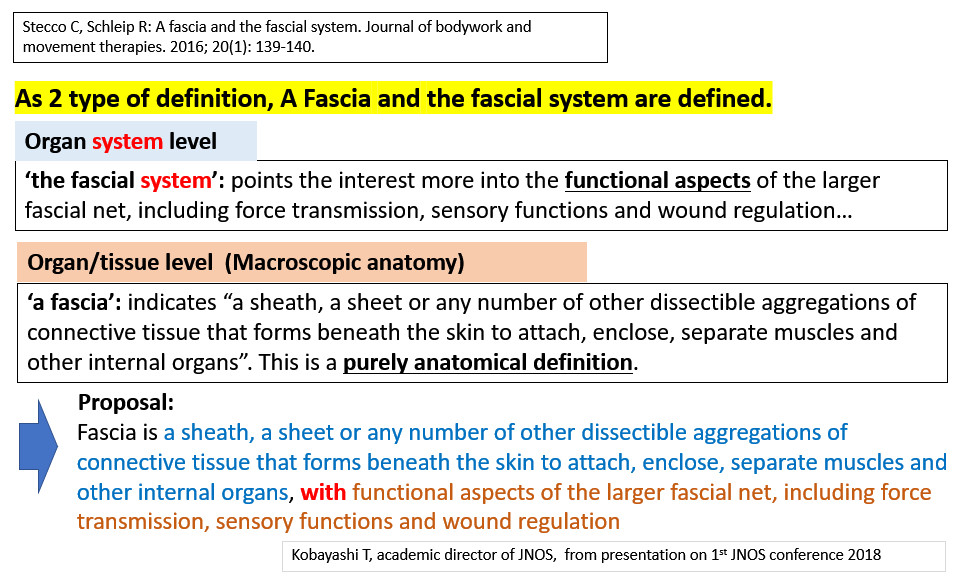
Today, 2 types of definitions, “A fascia” and “fascia system” are defined.
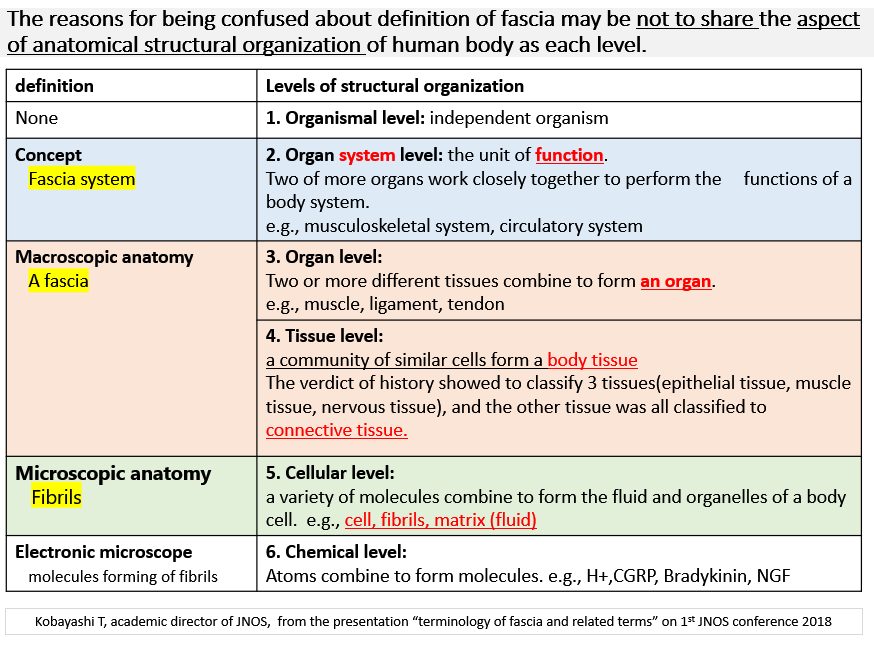
The reasons for being confused about the definition of fascia may be not to share the aspect of anatomical structural organization of human body as each level (below figure).
As the term of fascia, JNOS proposal for the new definition: “Macroscopic anatomical structures forming of fibers with the function of fascial network system (Terminology of JNOS, 1st edition, 2019 Mar)”: as each factor;
As the anatomy of fascia: macroscopic anatomical structures forming of fibrils
As the function of fascia: with the function of network
3.What are abnormal fasciae which cause any symptoms?
JNOS proposed the classification criteria for fascial pain syndrome (FPS) on July 1st, 2019.
3-1 FPS (fascial pain syndrome)
The sensory, motor, and autonomic symptoms caused by abnormal fascia. The specific fascia and a fascial group that causes the symptoms should be identified.
The classification criteria for fascial pain syndrome (FPS)
This classification criterion is made available when one or more apparent abnormal fascia is identified, which cannot be explained by another diagnosis. FPS is classified when all essential criteria are fulfilled and at least one more confirmatory observation is made. After FPS is classified, the precise intervention for abnormal fascia (e.g., ultrasound-guided intervention) is performed to relieve symptoms of FPS significantly (relief of restrictive range of motion and 75% or more of the pain intensity as per the criterion standard).
Classification criteria for FPS (JNOS July 1st, 2019)
- Essential Criteria
- Exquisite spot tenderness if the abnormal fascia is accessible
- Identification of high echoic strip-shaped lesions as stacking fascia as high-density, adhesive or cohesive fascia on ultrasound findings on/in the same tenderness spot
- Restriction of passive range of motion or painful limit to full passive stretch caused by abnormal fascia.
- Confirmatory Observations
- Low extensibility of fascia and/or sliding between fasciae caused by abnormal fascia.
- Visual, tactile or ultrasonographic identification of local twitch response induced by needle penetration of abnormal fascia
- Observation of increase of arterial pulse pressure near the abnormal fascia released by a procedure
- Patient’s recognition of current complaint induced by needle stimulation to abnormal fascia
3-2 Pathophysiologic terms of fascia
We here explain common words (It is planned to increase in the future).
- Adhesion: The meaning of adhesion is connecting between tissues not normally connected. Although the “strength” of the adhesion itself is not included in the original definition as terminology, different people have different images of adhesion strength in the situation that they imagine from their own experience. As another means that a fibrous band or structure by which parts abnormally adhere, adhesion is usually used in the nuances of “scar,” especially in some clinical settings.
- Cohesion: The historical meaning of Cohesion is “molecular attraction by which the particles of a body are united throughout the mass.” That is, as mentioned above, “union between similar plant parts or organs” as a tissue or organ, it means “a state where same or similar tissues are aggregated in one structure.” The strength of cohesion is also not included in the definition as same as that of adhesion.
- Stacking fasciae: hyperechoic strip-shaped lesions on ultrasound images. The word “stacking” originates from polyacrylamide gel electrophoresis. Caution: The ultrasound image of stacking fasciae tend NOT to be visualized due to optimization of ultrasound images, such as strong noise removal. F
In the case of fascia, especially deep fascia, which has a network structure as a three-dimensional structure between outer muscles, the term of “cohesion” could be more appropriate compared to that of “adhesion.”
4.Diagnosis/assessment of fascia
In clinical practice, it is crucial to assess the precise identification of the source of pain and exacerbating factors associated with patients’ symptoms, and the sharing of assessments for interprofessional collaboration (below figure).
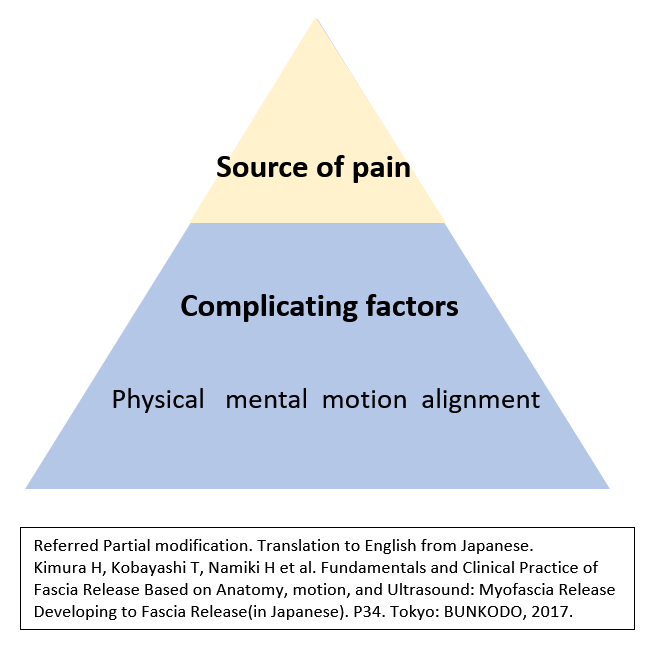 Physicians and therapists should be to perform a medical interview, physical examination (palpation, motion-analysis at pain motion, range of motion and special tests for orthopedic examination), and diagnostic imaging such as ultrasonography, based on various clinical methods including dermatomes and fasciatomes, pattern of referred pain, and clinical anatomy such as peripheral nerves (around/on/in them, e.g., perineurium, interfascicular epinerium, fibrils), vessels (around/on them), muscles (on/in them), tendons(on/in them), ligaments(on/in them), and fascia (including fibrils).
Physicians and therapists should be to perform a medical interview, physical examination (palpation, motion-analysis at pain motion, range of motion and special tests for orthopedic examination), and diagnostic imaging such as ultrasonography, based on various clinical methods including dermatomes and fasciatomes, pattern of referred pain, and clinical anatomy such as peripheral nerves (around/on/in them, e.g., perineurium, interfascicular epinerium, fibrils), vessels (around/on them), muscles (on/in them), tendons(on/in them), ligaments(on/in them), and fascia (including fibrils).
5.Therapy of fascia
5-1 Guide for selecting the type of treatment tequniques
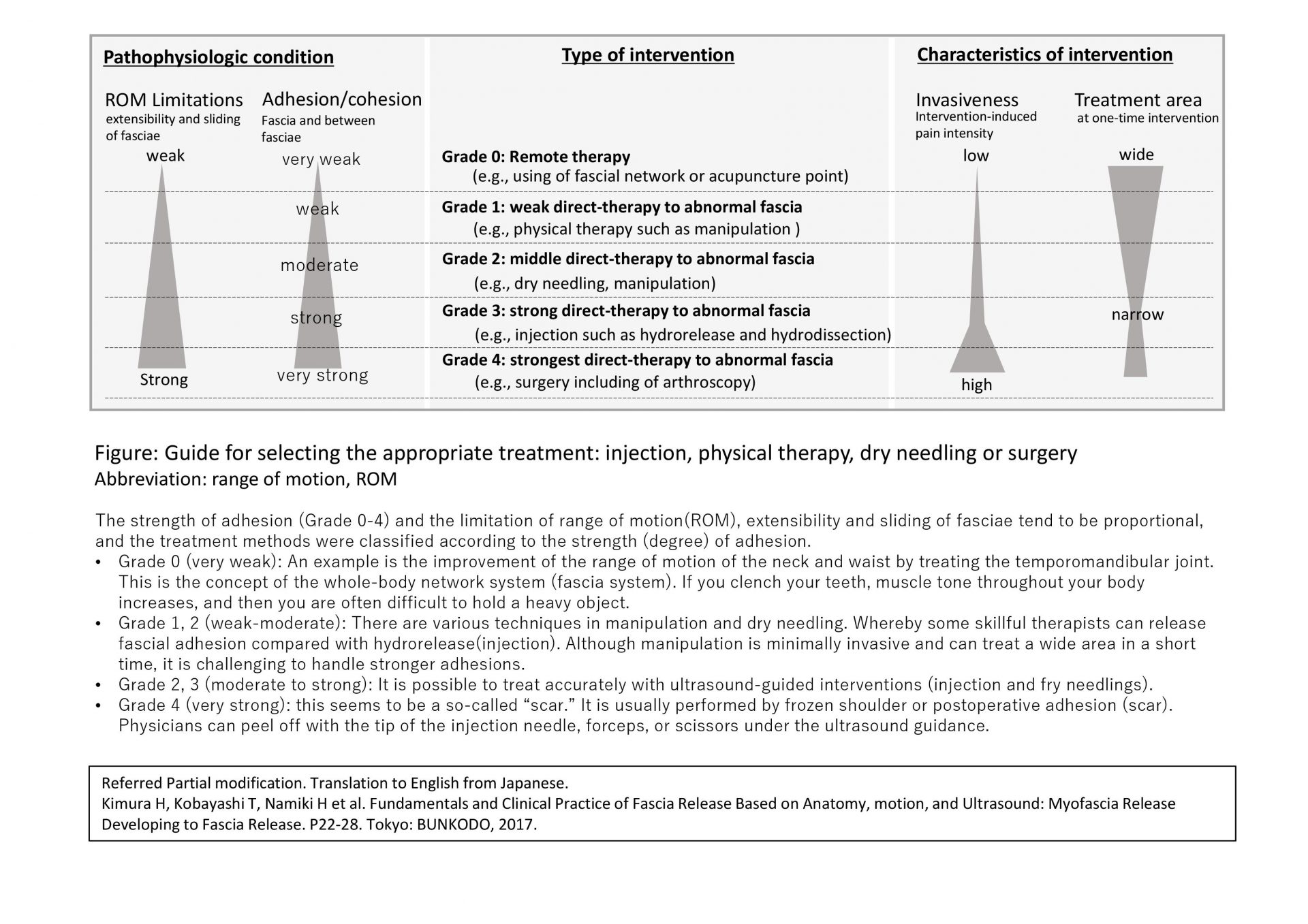
There are various theraputic techniqes for fascia to select or combinate physical therapy, manipulation, acupuncture/dry needling, injections and less invasive surgery.
5-1-1 How to use of SOLO therapeutic technique – Grading of Adhesions/Cohesions
We have proposed differentiation in the use of solo therapeutic technique, based on pathophysiologic conditions (range of motion, adhesion/cohesion of fascia) and characteristics of interventions (invasiveness and treatment area) (Below figure). For instance, broad and weak fascial adhesions can be treated with physical therapy, and strong adhesions can be treated with injections. Furthermore, each treatment may be performed alternately or in sequence.
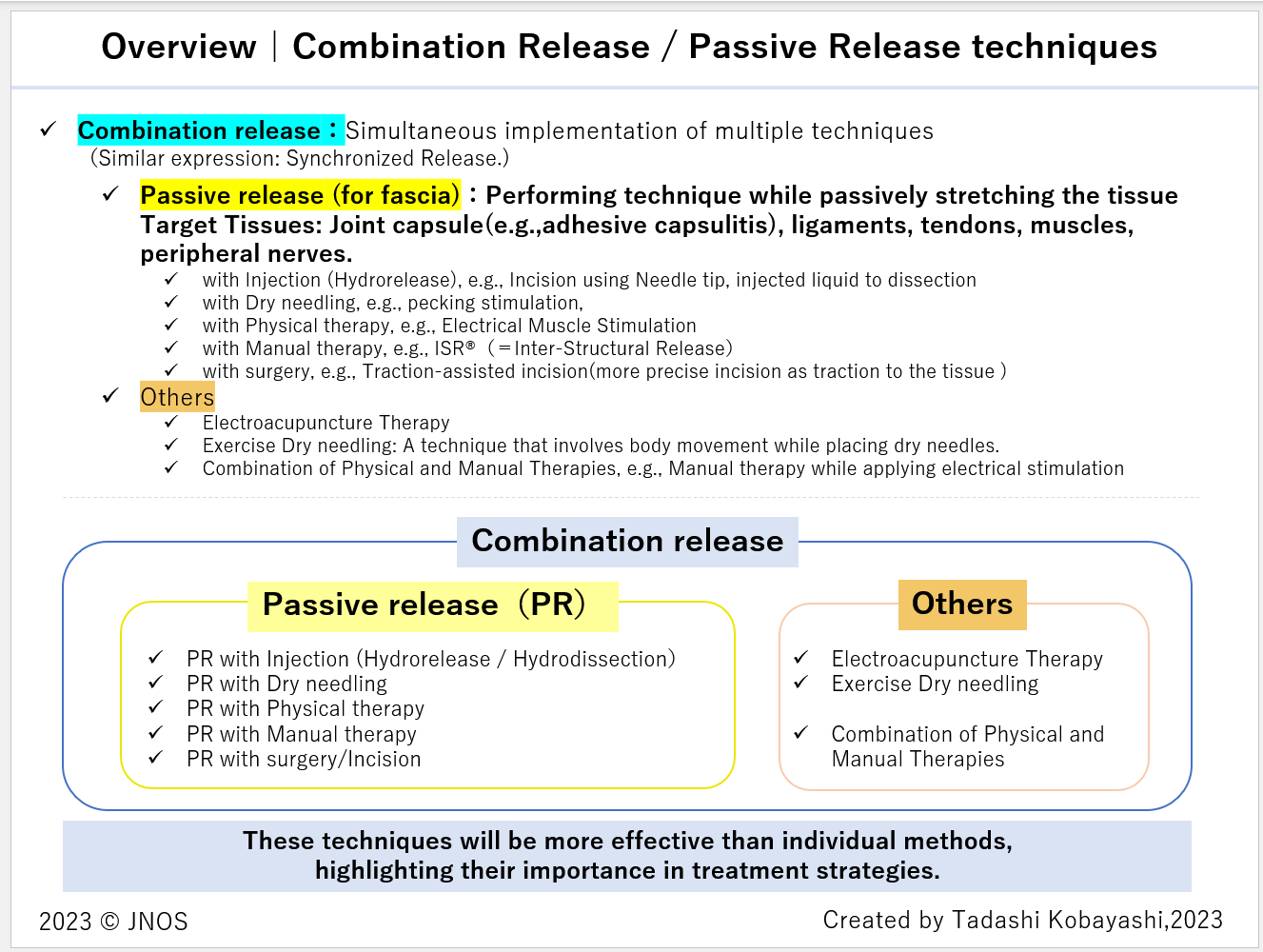
5-1-2 Combination release techniques : e.g., Fascia stretch test → Passive Release (with Hydrorelease)
Therapists practicing in this field likely realize that adding manual therapy after injections enhances the therapeutic effects. The decision to administer the injection (or acupuncture) first or opt for manual (or exercise) therapy depends largely on the medical institution or clinic and the therapist’s characteristics.
Musculoskeletal ultrasound enables both static and dynamic observations, the latter involving joint movement. The primary goals of dynamic observation include:
- Assessing the fascia’s extensibility and glide, observing the adhesions’ extent, and their changes before and after treatment.
- Observing the direction of muscle glide during joint movement and the muscle’s thickness during contraction.
- Visualizing muscle contractions to aid in the anatomical examination of muscles and surrounding tissues.
In 2018, Kimura and colleagues identified the “tight fascia sign” on ultrasound images through dynamic observation, which indicates a taut-like movement. When the range of motion is restricted, checking for the tight fascia sign helps evaluate decreased fascia extensibility and glide, or its shortened state, thus aiding in selecting treatment areas. Injecting in the presence of the tight fascia sign can achieve different therapeutic effects than performing manual and injection therapies separately. Dr.Kimura and others, in 2019, named the technique “Passive Release technique (with hydrorelease),” which involves intervening Hydrorelease in a passively extensed fascia (e.g., maximally passive Range of motion such as capsle, ligament, tendon, muscle, peripheral nerve). This technique can be interpreted as a simultaneous implementation of “injection therapy + manual therapy.” Notably, injecting into a tensed fascia, especially when aiming to improve range of motion, tends to yield greater improvement than injecting into a relaxed fascia. This action detaches the tensed fascia and peels off the surrounding tissues, gradually relaxing the tissue. It is crucial for the assistant to control the patient’s joint range of motion in line with the expanding range, ensuring the fascia’s tension is maintained.
Additionally, we recommend the “Fascia Stretch Test” as an evaluation method that leverages the stretching of fascia to make it easier to apply manual stress, thereby clarifying tender points. Traditionally, tenderness often resulted in false negatives when there was no firm tissue (e.g., bone) at the posterior aspect. By stretching the target tissues (skin, subcutaneous tissue, muscle fascia, ligaments, tendons, peripheral nerves, etc.), a technique has been employed to more easily identify tenderness. For example, the Nerve Stretch Test (Nerve Tension Test) not only involves traction of peripheral nerves but also evaluates the tender points of the peripheral nerves under traction to determine the specific site of pain origination (manual evaluation of gliding is also often performed simultaneously). This generalized evaluation method for fascia was named the “Fascia Stretch Test” by Hiroaki Kimura and Tadashi Kobayashi in October 2023.
As the effectiveness of passive release continues to be validated, evaluations based on the aforementioned Fascia Stretch Test and Tight Fascia Sign are becoming established as part of the sequence of fascia treatment. This integration allows for evaluation and treatment to be carried out seamlessly. Consequently, the collaboration among multiple professions for simultaneous evaluation and treatment has become significantly smoother and more effective.
Evaluation and Treatment of Fascial Pain Syndrome (FPS)
= Fascia Stretch Test (+ Tight Fascia Sign) → Passive Release
In 2021, our book introduced the passive release technique, and since then, there has been ongoing clinical refinement.
(in Japanese) Hiroaki Kimura, Tadashi Kobayashi, Hirofumi Namiki /eds. Fundamentals and Clinical Practice of Fascia Release based on Anatomy, Motion, and Ultrasound: 2nd edition- Focusing on Hydrorelease of Fascia. BUNKODO, 2021, p.111
In June 2023, Dr. H.Kimura and Dr. T.Kobayashi introduced the passive release of the shoulder joint, comparing it with silent manipulation (a manipulative technique performed under brachial plexus block that can be done in an outpatient setting) (link).
In the Expert Seminar of September 2023 (link) and the Webinar of October 2023 (link), they introduced the passive release for the hip joint, along with tips for the technique.
In November 2023, the effectiveness of various simultaneous therapeutic techniques, such as electroacupuncture, EMS treatment (electrical stimulation therapy) combined with manual therapy, was reported at the 6th JNOS Academic Conference and the 4th Japan Fascia Conference (link). Following this, under the leadership of Tada Kobayashi, Director of the JNOS Academic Bureau, the framework of simultaneous release techniques was examined and organized as follows.
5-2 What is fascia hydrorelease?
5-2-1 Definition of fascia hydrorelease
- Fascia hydrorelease (Hydrorelease of fascia) is defined as a injection technique for the release (separation and relaxation) of abnormal fasciae to improve the extensibility and sliding in addition to having analgesic effects.
- The technique of ultrasound-guided fascia hydrorelease is a injection technique for the release of abnormal fasciae as hyperechoic strip-shaped lesions on ultrasound images, akin to peeling off thin stacking papers and separating fasciae themselves.
5-2-2 History of fascia hydrorelease(fascia HR)
In 2008, Dr. Hiroaki Kimura et al. proposed interfascial block with local anesthetic as a novel treatment procedure for MPS(myofascial pain syndrome) (Kimura, H. 2008. Interfascial injection with a local anesthesia (in Japanese). 2nd conference of Japanese society for the study of myofascial pain syndrome (JMPS). Tokyo.).
In 2012, Kimura reported that the injection of physiological saline instead of a local anesthetic could relieve the symptoms caused by abnormal fascia (Kimura H. 2012. SUKIMA block (interfascial block) with physiological saline: new procedure for myofascial pain syndrome. In: 10th conference of Japanese Society for the Study of Myofascial Pain Syndrome).
In June 2014, Kimura devised a novel procedure termed “ultrasound-guided myofascial release injection”, which was defined as a technique for the release (separation in structural view and relaxation in functional view) of stacking fasciae as hyperechoic strip-shaped lesions on ultrasound images, akin to peeling off thin stacking papers and separating fasciae themselves (Kimura H. 2014. A new injection technique of ultrasound-guided myofascial release (in Japanese). In: 13th conference of Japanese Society for the study of Myofascial Pain Syndrome.).
The word “stacking” originates from polyacrylamide gel electrophoresis. This injection aims to improve the extensibility of fasciae or to slide between fasciae in addition to having analgesic effects.
In 2015, the target of treatment expanded from myofascia to fascia (including deep fascia, myofascia, paraneural sheath, tendon, ligament, retinaculum, and fat pad) (Kimura H. 2015. Myofascial release developing to fascial release (in Japanese). In: 15th conference of Japanese Society for the study of Myofascial Pain Syndrome.).
In 2016, Kobayashi et al. reported two double-blind, randomized controlled studies comparing three types of solutions (physiological saline, local anesthetic, and bicarbonate Ringer’s solution) on ultrasound-guided interfascial (fascial release injection for deep fascia) injection for MPS (Kobayashi T, et al. Effects of interfascial injection of bicarbonated Ringer’s solution, physiological saline and local anesthetic under ultrasonography for myofascial pain syndrome -Two prospective, randomized, double-blinded trials. J Juzen Med Soc.2016. 125(2):40-9).
Fascia release includes various therapeutic techniques such as physical therapy, dry needling, injections and less invasive surgery.
In March 2017, fascia hydrorelease (fascia HR) was an injection therapy using physiological saline or various solutions without local anesthetics that targets various types of fascia. In March 2017, 4 Japanese, Dr. Tadashi Kobayashi, Dr. Hiroaki Kimura, Dr. Yoshihiko Shiraishi and Dr. Hiroshi Minagawa, adopted the term “fascia hydrorelease” for fascial release injections.
5-3 The difference between hydrorelease (HR) and hydrodissection (HD)
HD and HR are similar in that local anesthetics are not employed. The fundamental differences between HD and HR are shown in the below table and figure.
Presumptive action mechinism of HR of fascia are as belows:
- Rehydration (electrolyte such as Na+, Cl- ) of matrix
- Washing effect of pain substances
- Mechanical and chemical effects of fascia and extracellular matrix
- Stimulation of free nerve endings, other sensory receptor
- Improvement of extensibility of fascia and sliding between fasciae
- Improvement of abnormal blood flow (e.g, shunt blood flow)
5-4 Comparision of targets and ultrasound signs between Hydrorelease(HR), Hydrodissection(HD), and Peripheral nerve block
Below is comparision of targets and ultrasound signs between Hydrorelease(HR), Hydrodissection(HD), and Peripheral nerve block.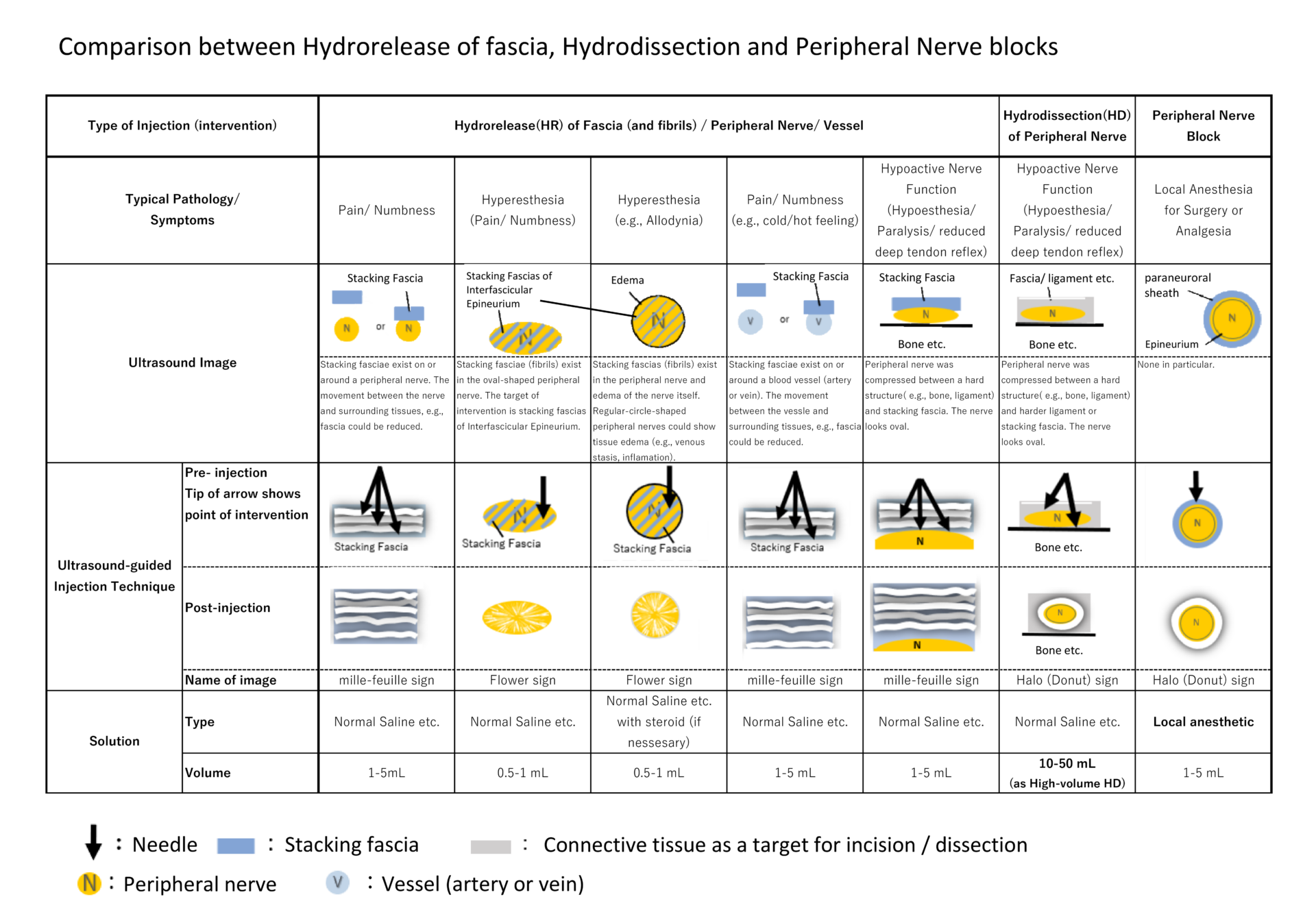
Ref: (in Japanese) Kimura H, Kobayashi T, Namiki H/eds. Fundamentals and Clinical Practice of Fascia Release based on Anatomy, Motion, and Ultrasound: 2nd edition- Focusing on Hydrorelease of Fascia. BUNKODO, 2021, p.100, table 1. all pages of 340. On YouTube of JNOS, we introduce this book as JNOS webinars(First movie、Second movie)
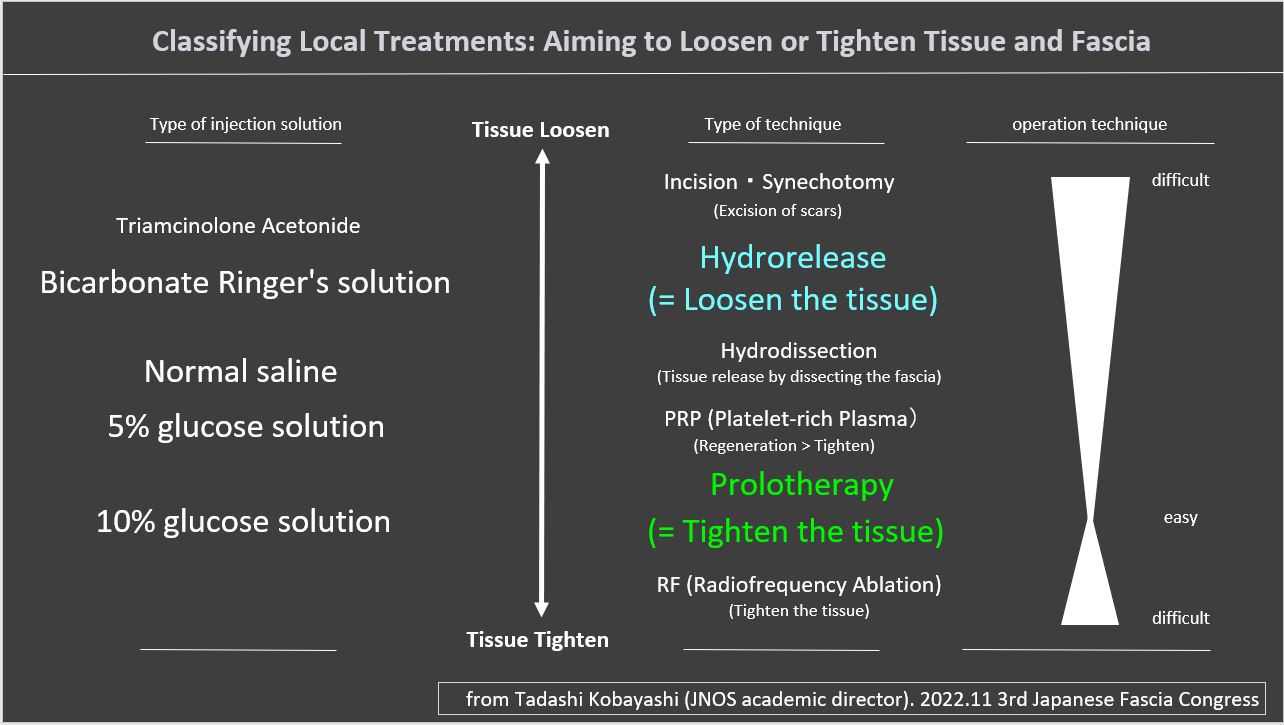
5-5 Classifying Local Treatments: Aiming to Loosen or Tighten Tissue and Fascia
We suggest that the idea of classifying local treatments is to determine whether they aim to loosen or tighten the tissue and fascia. Tadashi Kobayashi (JNOS academic director) proposed on 2022.11 3rd Japanese Fascia Congress & 5th JNOS academic conference (link, Movie: Japanese language)
5-6 Hydrorelease of fibrils as of fascia, into a peripheral nerve
As shown above 5-4, we shed light on useful technique, hydrorelease of fibrils as of fascia, into a peripheral nerve.However, the injections into the peripheral nerves do not correspond to the previously mentioned “A fascia” (a term in macroscopic anatomy). On the other hand, the epineurium and the perineurium exhibit tissue continuity. This is similar to the relationship between the epimysium as outer muscle and the fibrous tissue inner of muscle. The inner are part of the fascia system, but they are not included in the A fascia. At this level, I have suggested that another structural name, fibrils, is necessary.
This technique involves injections into the a peripheral nerve, aiming to treat the epineurium and the fascia (more precisely, fibrils) containing the perineurium. Upon injecting the solution into the epineurium, it instantaneously (in milliseconds) spreads throughout the peripheral nerve, which can be observed as a “flower sign” on Ultrasound image. (July 2020, Hiroaki Kimura, Tadashi Kobayashi, JNOS Webiner).
Comparing injections into the peripheral nerves and injections around the peripheral nerves, the former has been reported to have higher short-term efficacy, with no significant differences in complications (Christian W.A. et al. Radiology, 2001). However, this technique carries a risk of nerve damage, and its indiscriminate use is discouraged in the field of anesthesiology. Therefore, it should be considered only for intractable cases that do not improve with other treatments, and its application should be carefully assessed.
In the past, “blind” peripheral nerve blocks without ultrasound or X-ray were performed based on the indicator of “radiating pain” caused by the block needle tip contacting the nerve itself. However, “radiating pain” did not necessarily lead to nerve damage (clinical sequelae of nerve damage). Even with more precise injection techniques, such as ultrasound-guided injections of local anesthetics into peripheral nerves, nerve damage did not always occur (Paul E. Bigeleisen. ANESTHESIOLOGY. 2006). Nevertheless, reducing the risk associated with the procedure is essential. In our association,JNOS, when performing injections into peripheral nerves for the purpose of hydrorelease (HR) of fibrils as of the part of fascia, it is desirable to avoid the use of local anesthetics, as the goal is not to achieve a “block”. Although a 2017 systematic review reported no clear causal relationship between the continuous administration of local anesthetics around peripheral nerves and neurotoxicity (Sondekoppam RV et al. Anesthesia & Analgesia. 2017), clinical concerns remain.
Furthermore, it is important to use very fine needles, such as 27, 30 or 32 guage, and to consider the orientation of the bevel during insertion. Attention should also be paid to the type of injection needle used. For example, the “Pencil point type” needle has been suggested to be safer than the “Quincke type” needle for procedures involving nerve roots (Takahashi et al., Pain Clinic, 2010). With these precautions in place, it should be performed the procedure without causing radiating pain even when the needle is inserted into the epineurium. In cases where peripheral nerve edema is observed, a small amount of corticosteroid might be cautiously used, but the indication must be selected with highly-advanced option.
5-7 Specific examples of ultrasound-guided fascia hydrorelease
Below are some typical techniques for ultrasound-guided fascia hydrorelease(injections)
Case 1: Intervertebral joint (capsular ligaments) / multifidus muscle / deep fascia
Case 2: Subacromial bursa (supraspinatus muscle/subacromial bursa/deltoid muscle/deep fascia)
Case 3: Trapezius muscle/deep fascia/supraspinatus muscle (include: dorsal scapular artery /accessory nerve / fat tissue)
6. Message for multi-medical professionals
Currently, fascia’s academic fields include various medical systems such as Western medicine, Oriental medicine, and alternative medicine, or comprehensive treatment techniques such as surgery, arthroscopy, injection, acupuncture, manipulative therapy, physical therapy, and exercise therapy. It is attracting attention as a new field to promote understanding.
In the non-surgical orthopedic field, various treatment techniques such as local treatment, exercise therapy, life movement guidance, pharmacotherapy, and cognitive behavioral therapy are handled in a complementary manner in many occupations. JNOS hopes that fascia is logically integrated with traditional Western medicine to deepen medicine further.
7. Further Information
- (in English) Tadashi Kobayashi, Hiroaki Kimura, Yoshihiro Zenita, Hidetaka Imagita. 7.23 Hydrorelease of Fascia. Editors; Robert Schleip, Carla Stecco, Mark Driscoll, Peter Huijing. Fascia: The Tensional Network of the Human Body, 2nd Edition 2021 ELSEVIER p.609-617 [link of ELSEVIER]
- (in Japanese) Hiroaki Kimura, Tadashi Kobayashi, Hirofumi Namiki /eds. Fundamentals and Clinical Practice of Fascia Release based on Anatomy, Motion, and Ultrasound: 2nd edition- Focusing on Hydrorelease of Fascia. BUNKODO, 2021, p.100, table 1. all pages of 340. [link of BUNKODO] On YouTube of JNOS, we introduce this book as JNOS webinars(First movie、Second movie)